|
CASE REPORT |
https://doi.org/10.5005/jp-journals-10070-7096
|
An Interesting Case of Pancytopenia
1,4Department of Oncology, Peerless Hospital and BK Roy Research Centre, Kolkata, West Bengal, India
2Laboratory Services, Peerless Hospital and BK Roy Research Centre, Kolkata, West Bengal, India
3Department of Microbiology, Peerless Hospital and BK Roy Research Centre, Kolkata, West Bengal, India
5Department of General Medicine, Peerless Hospital and BK Roy Research Centre, Kolkata, West Bengal, India
Corresponding Author: Madhuchanda Kar, Department of Oncology, Peerless Hospital and BK Roy Research Centre, Kolkata, West Bengal, India, Phone: +91 9830155915, e-mail: apiwbb@gmail.com
How to cite this article: Kar M, Sanyal S, Chaudhuri BN, et al. An Interesting Case of Pancytopenia. Bengal Physician Journal 2022;9(3):75–76.
Source of support: Nil
Conflict of interest: Dr. Madhuchanda Kar is associated as the Editorial Board Member of this journal and this manuscript was subjected to this journal’s standard review procedures, with this peer review handled independently of the Editor-in-Chief and his/her research group.
Received on: 01 December 2022; Accepted on: 26 December 2022; Published on: 06 January 2023
ABSTRACT
This is a case report of an immunocompromised adult female presented with fever and reddish-colored spots all over the body along with bilateral swelling of parotid and submandibular glands. Hematological parameters revealed pancytopenia, and she was diagnosed with disseminated histoplasmosis by bone marrow trephine biopsy. The patient was treated with antimicrobials and other supportive therapy, but she rapidly deteriorated and succumbed to the underlying bone marrow infiltration and failure.
Keywords: Histoplasmosis, Immunocompromised, Pancytopenia.
INTRODUCTION
Pancytopenia is defined as a decrease in the red blood cell, white blood cell, and platelet count.1 Pancytopenia is not a disease but a common entity caused by different underlying clinical conditions, including infections, autoimmune disease, genetic abnormality, nutritional deficiency, and some malignancy. Individual laboratories typically have their own reference ranges for hemoglobin/hematocrit, white blood cell, and platelet counts. The standard cutoff for pancytopenia as published by WHO is as follows:2
Red blood cell – hemoglobin less than 12 gm/dL for women (non-pregnant) and less than 13 gm/dL for men.
White blood cells – leukocyte count less than 4000/µL. (absolute neutrophil counts < 1800/µL).
Platelets – platelet count less than 150000/µL.
Histoplasmosis is a systemic fungal infection caused by the dimorphic fungus Histoplasma capsulatum. Histoplasma is a widely distributed fungus, cosmopolitan in distribution except for Antarctica, but mostly found near river valleys. In India, histoplasmosis mostly occurs in small areas of West Bengal and Assam, Western parts of India, The Gangetic Plains, and a few sporadic cases from southern and northern Indian states.3 Histoplasma is a dimorphic fungus, it can switch from a filamentous growth form (mold-like) in the natural habitat to a small budding yeast form (spherical) in warm-blooded animal hosts.4 Infection occurs by inhalation of spores present in soils contaminated by bird or bat droppings.5 The clinical presentations are variable, which may present as asymptomatic to disseminated forms, depending on the immune status of the host and the amount and type of inoculums.
CASE DESCRIPTION
A 56-year-old female patient, homemaker by occupation, residing in Agartala, presented with complaints of fever, reddish spots all over the body, and hard palate for the last 1 month. The patient also complained of bilateral swelling of the cheeks for the last 7 days. The patient had severe anorexia and fatigue for the last 1 month. No other specific symptoms were present.
On general examination, the patient was febrile, her BP was 130/80 mm of Hg, and her pulse rate was 108 bpm. She had severe anemia, petechiae, and extensive ecchymosis over different parts of the body. Mucosal hemorrhage was noted over the hard palate along with severe oral thrush. On palpation, swelling was noted over bilateral parotid and submandibular glands. There was no icterus, cyanosis, or clubbing. Systemic examination showed no organomegaly or palpable mass per abdomen.
Investigations like complete blood count revealed Hb – 5.6 gm/dL, TLC – 1000/µL, and platelet count of 24000/µL. Dengue NS1, malaria dual antigen, COVID-19 (RT-PCR), and HIV along with other routine viral markers were all negative. Chest X-ray (Fig. 1) was done that revealed right-sided pleural effusion and large consolidation in the upper and middle lobe of the right lung. HRCT thorax (Fig. 2) was done, which revealed large area consolidation in the right upper and middle lobes having perilesional ground glass opacity and multifocal interstitial nodular deposits along with multiple mediastinal lymphadenopathies. Bone marrow aspiration was done which revealed grossly hypoplastic marrow with relative increase in plasma cells >10%, reticulum cells, and mast cells were within normal limits. Bone marrow trephine biopsy revealed granuloma and nonhematopoietic foreign cells and macrophages having small round intracytoplasmic PAS-positive fungal bodies (Fig. 3). Gomori methenamine silver staining (Fig. 4) was done, which revealed black-colored yeast-like cells of H. capsulatum. The patient was started on broad-spectrum antibiotics (Meropenem in slandered dose), and later liposomal Amphotericin B was started. However, soon after this, the patient succumbed to persistent bone marrow failure.
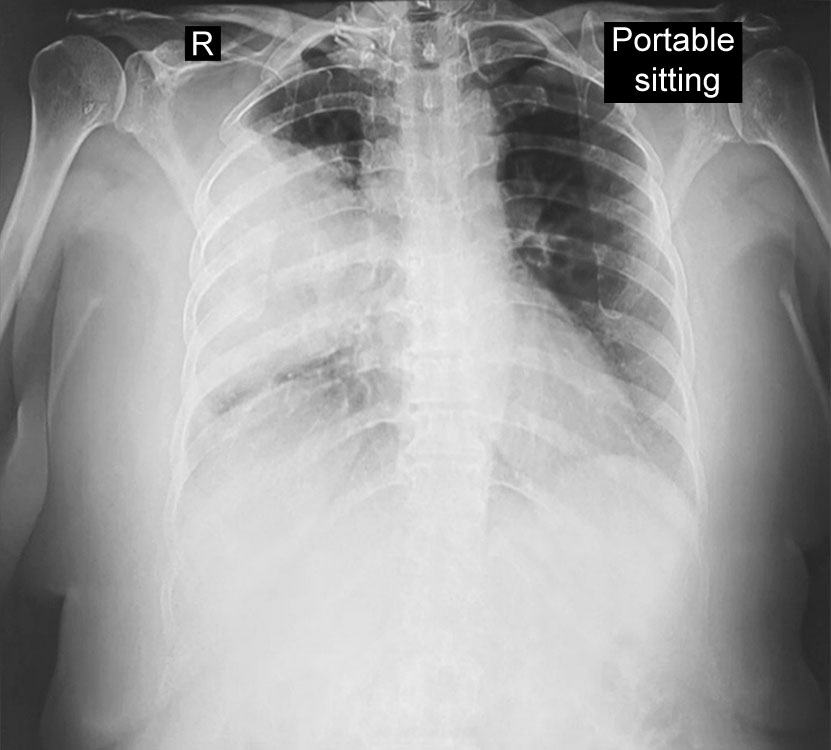
Fig. 1: Chest X-ray on sitting position showing right-sided pleural effusion along with consolidation

Fig. 2: HRCT of thorax showing a large area of consolidation and multifocal interstitial nodular deposits of the right upper and middle lobes of the lung

Fig. 3: PAS-stained bone marrow biopsy
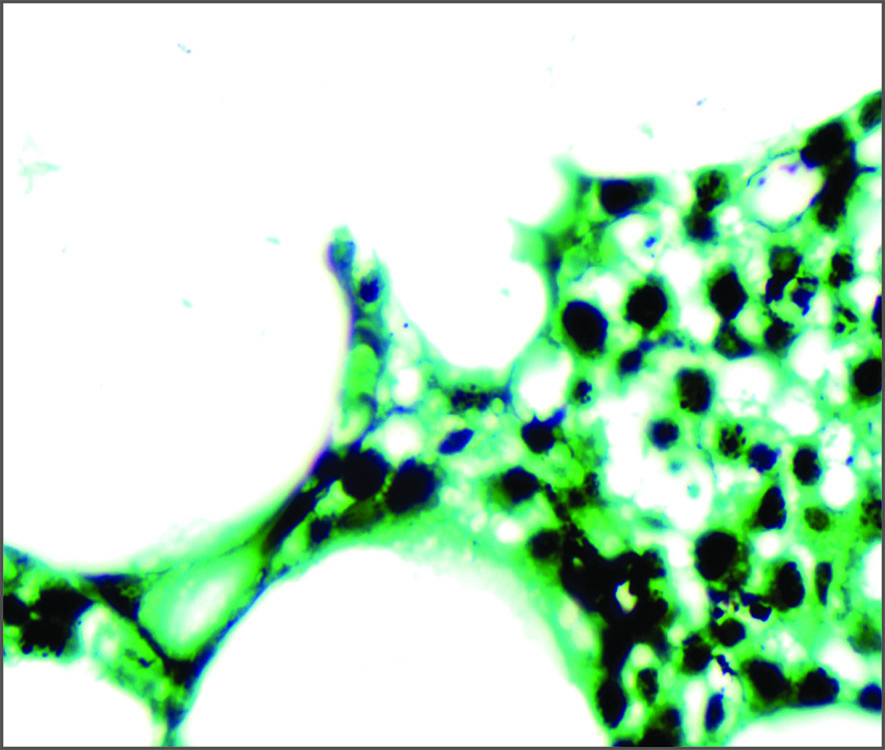
Fig. 4: Gomori methenamine silver staining of bone marrow showing black-colored yeast-like cells of histoplasma
DISCUSSION
Histoplasma capsulatum is the etiologic agent of histoplasmosis. Histoplasmosis is the most prevalent endemic mycosis found in North America, particularly in the Ohio and Mississippi River basins. Although this fungal infection has been reported worldwide, its endemicity is high in North America and in certain parts of Central and South America, Africa, and Asia. In immunocompetent individuals with low-level exposure, it is mostly present in asymptomatic or self-limited form, but in patients with impaired cellular immunity, the infection can disseminate to different systems, including the reticuloendothelial system.6 Progressive disseminated histoplasmosis (PDH) can affect multiple organs, most commonly the lungs, bone marrow, liver, spleen, and adrenal glands, and in some cases, mucocutaneous membranes can also be affected.7 Progressive disseminated histoplasmosis can be seen in immunocompromised individuals, who account for about 70% of the cases out of which only 4% involve the bone marrow.8
REFERENCES
1. Chiravuri S, Jesus OD. Pancytopenia. StatPearls. StatPearls Publishing, 2022. http://www.ncbi.nlm.nih.gov/books/NBK563146/.
2. UpToDate. https://www.uptodate.com/contents/approach-to-the-adult-with-pancytopenia#H115856 (Accessed 11 December, 2022).
3. Mahajan VK, Raina RK, Singh S, et al. Case report: Histoplasmosis in Himachal Pradesh (India): An emerging endemic focus. Am J Trop Med Hyg 2017;97(6):1749–1756. DOI: 10.4269/ajtmh.17-0432.
4. Histoplasma capsulatum. Wikipedia. 9 August, 2022. https://en.wikipedia.org/w/index.php?title=Histoplasma_capsulatum&oldid=1103508252.
5. Evrard S, Caprasse P, Gavage P, et al. Disseminated histoplasmosis: Case report and review of the literature. Acta Clin Belg 2018;73(5):356–363. DOI: 10.1080/17843286.2017.1376454.
6. Samaddar A, Sharma A, Ph AK, et al. Disseminated histoplasmosis in immunocompetent patients from an arid zone in Western India: A case series. Med Mycol Case Rep 2019;25:49–52. DOI: 10.1016/j.mmcr.2019.07.012.
7. Jameson JL, Fauci AS, Kasper DL, et al. Harrison’s Principles of Internal Medicine. 20th edition, McGraw-Hill Education, 2018.
8. Lugo A, Adjapong A, Ahmad W. Histoplasmosis: Fever of unknown origin disseminated to bone marrow.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.