|
CORRESPONDENCE |
https://doi.org/10.5005/jp-journals-10070-7090
|
Diabetic Pyomyositis: An Unusual Cause of Painful Thigh
1–7Department of Neurology, Stanley Medical College, Chennai, Tamil Nadu, India
Corresponding Author: Mugundhan Krishnan, Department of Neurology, Stanley Medical College, Chennai, Tamil Nadu, India, Phone: +91 9840444280, e-mail: mugundhan69@gmail.com
How to cite this article: Krishnan M, Kamalakannan M, Budumuru U, et al. Diabetic Pyomyositis: An Unusual Cause of Painful Thigh. Bengal Physician Journal 2022;9(3):77–79.
Source of support: Nil
Conflict of interest: None
Received on: 16 March 2022; Accepted on: 13 November 2022; Published on: 06 January 2023
ABSTRACT
Pyomyositis is defined as the pyogenic infection of skeletal muscle, which leads to the formation of an abscess. It is difficult to diagnose in its early course, due to poor localizing signs and vague presentation. Diagnosing pyomyositis needs a high index of suspicion. Any delay in diagnosis will lead to sepsis, compartment syndrome, and ultimately death. We describe here a case of pyomyositis of the left thigh, with a relatively non-specific presentation, who was successfully managed with antibiotics and aspiration of pus.
Keywords: Lumbosacral plexopathy, Osteomyelitis, Pyomyositis, Thrombophlebitis.
INTRODUCTION
Pyomyositis is defined as the pyogenic infection of skeletal muscle, which leads to the formation of an abscess. Skeletal muscles are usually resistant to infections. However, the infection can occur if the predisposing factors are present.1 It is difficult to diagnose in its early course, due to poor localizing signs and vague presentation. In the initial stage, the differential diagnosis is muscle hematoma, muscle rupture, musculoskeletal aches, thrombophlebitis, deep venous thrombosis, and muscle infarction. Any delay in diagnosis will lead to sepsis, compartment syndrome, and eventually death. Long-term sequelae will include muscle scarring, and osteomyelitis causing prolonged hospitalization and significant functional impairment. We are reporting a case of a diabetic patient who came with a painful thigh with relatively non-specific presentation and eventually was diagnosed with pyomyositis. Because of its rarity and ambiguous presentation, we should have heightened suspicion of it.
CASE DESCRIPTION
A 60-year-old gentleman, who is hypertensive and diabetic, presented with left thigh pain for 1 month, followed by difficulty in walking for 2 weeks. Over the next 2 weeks, he developed proximal muscle weakness in the left lower limb. There was no history of fever, trauma, localized swelling, loss of weight, or appetite. Examination showed the proximal weakness of the left thigh (MRC grade 3/5) associated with pain and absent knee and ankle reflexes. There was no sensory deficit and he had an antalgic gait. There was no muscle wasting noted. Minimal tenderness was present on deep palpation, however, there was no erythema or induration. His laboratory investigations were unremarkable except for raised blood sugars, which were managed with insulin. Serology for HIV, HBV, and HCV was negative. Ultrasound of the left thigh did not show any local collection. Serum CPK level was normal. A clinical diagnosis of diabetic lumbosacral plexopathy was made. The nerve conduction study and Doppler study of the lower limb were normal. The magnetic resonance imaging (MRI) Lumbosacral spine along with the plexus did not reveal any abnormality except for minimal disc disease at L3–L4 and L4–L5 levels.
The pain in his left thigh gradually worsened over the next week, and the power in the proximal left thigh worsened to 1/5. Examination at this point revealed minimal induration in the medial aspect of the thigh and there was severe tenderness on palpation, however, there was no erythema or warmth. Repeat ultrasound showed two ill-defined hypoechoic collections of size 4 cm × 3 cm × 4 cm and 5 cm × 4 cm × 6 cm in the proximal anteromedial aspect of the left thigh in the deep intramuscular plane (Fig. 1). The MRI of the left thigh showed multiple intramuscular abscesses of the left thigh, involving the entire muscle bulk of gracilis, adductor longus, and brevis with surrounding subcutaneous edema and fascial hyperintensity (Fig. 2). Ultrasound-guided (USG) aspiration of the collection-revealed pus (Fig. 3), which on laboratory examination, showed low sugar value, protein of 1.6 gm/dL, LDH-2857 U/L, 300 cells/mm3, neutrophilic predominance 80%. Cytology showed sheets of neutrophils and few lymphocytes in a necrotic background suggestive of abscess–acute inflammatory pathology. Tests for TB-AFB stain and CBNAAT were negative. Pus culture grew Staphylococcus aureus – sensitive to cloxacillin. The blood culture was sterile. The CT abdomen did not reveal any intra-abdominal collection. Ultrasound-guided aspiration of around 20–25 mL of pus was done twice and he was treated with parenteral antibiotics, following which pain was reduced and power improved so that he could walk with support. A follow-up scan done a week later showed the resolution of the abscess.
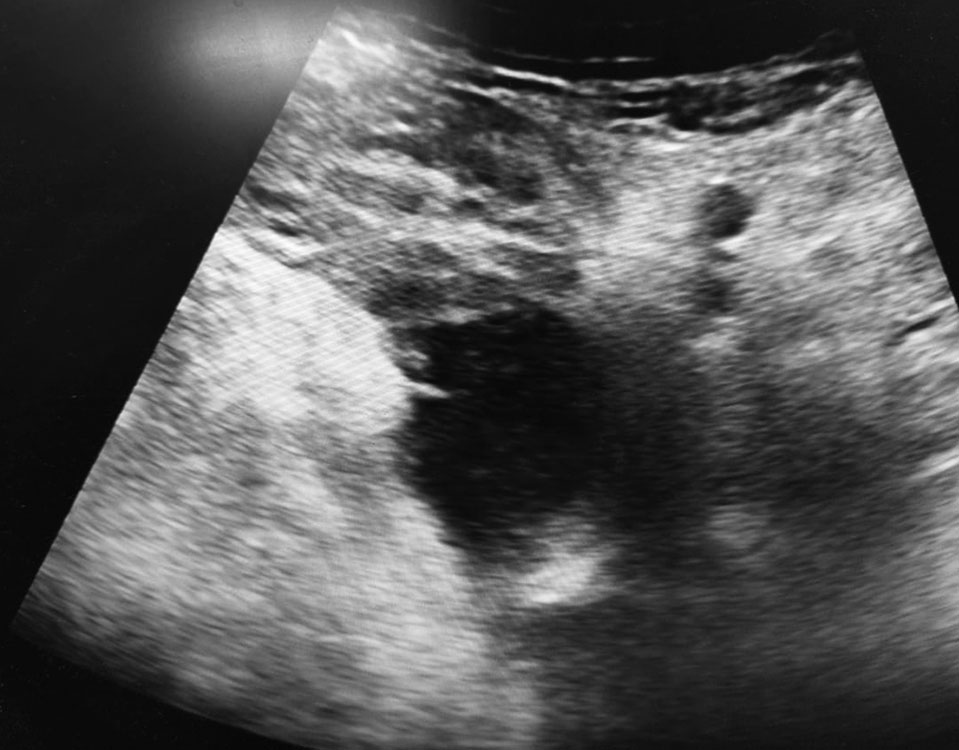
Fig. 1: The USG left thigh showing hypoechoic collection in deep
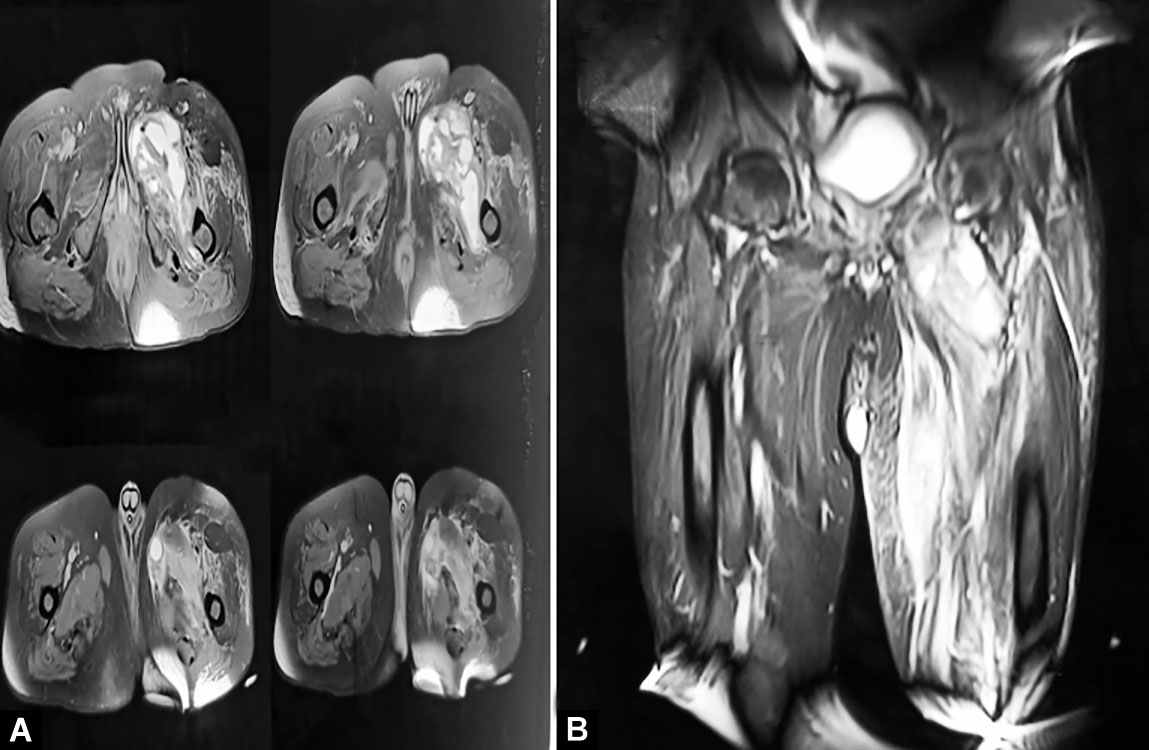
Figs 2A and B: The MRI thigh showing multiple intramuscular abscesses of left thigh, involving entire muscle bulk of gracilis, adductor longus and brevis with surrounding subcutaneous edema and fascial hyperintensity
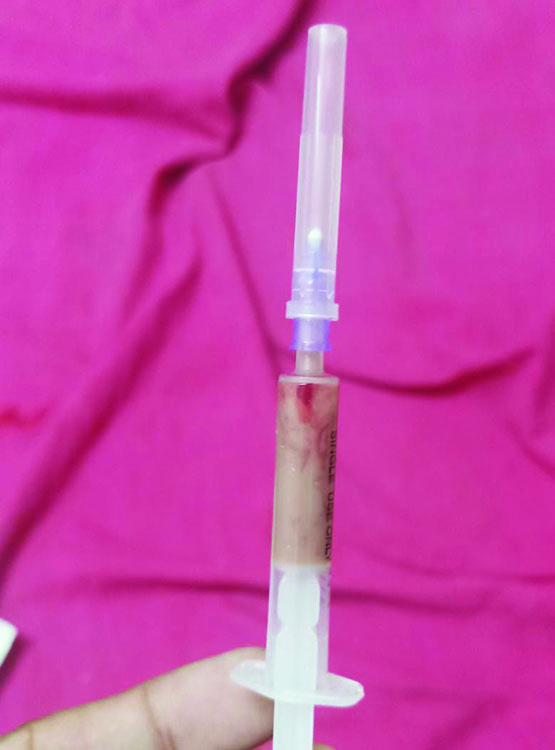
Fig. 3: The USG-guided aspiration of the collection showing pus
DISCUSSION
Pyomyositis is the bacterial infection of skeletal muscles presenting with fewer clinical signs and symptoms in the initial stages. Muscles commonly affected are the quadriceps, gluteus, and iliopsoas. Staphylococcus aureus is found to be the causative organism in over 75% of the cases.2 There are three stages as follows: First is an invasive stage, where there will be cramps and pain in the affected area, along with fever. It is actually 1–2 weeks before the accurate diagnosis is made. There will be woody consistency of the underlying muscle, but the clinical signs are minimal or can also be absent, similar to our case. There will not be fluctuation since the abscesses are very deep-seated in the muscles. The absence of external dermatological manifestations in the early stages makes this a challenging diagnosis.3 Hence, pyomyositis is usually missed during the early stages.3 Also, MRI is preferred to diagnose it at the earlier stage. Stage 2 involves the formation of muscle abscesses. Clinical features are more apparent in this stage and MRI shows ill-defined muscle enlargement and fluid collection will be seen as a hyperintense signal on T2 weighted images.2 If pyomyositis is not treated now, it progresses to stage 3 where the patient will develop septic shock and signs of sepsis.
Laboratory findings in pyomyositis are not specific. Leucocytosis and elevated ESR and CRP are observed, although not seen in every patient. Aldolase and creatinine kinase and aldolase levels are usually normal, as in our case. Blood cultures are positive only in 5–20% of cases, while pus culture has a yield of 70–85%. CT Abdomen is done to rule out intra-abdominal abscess as it can lead to secondary thigh abscess.1 The MRI also helps to study the adjacent structures such as bones, soft tissue, and joints. It also helps in differentiating pyomyositis from osteoarthritis, septic arthritis of the hip, osteomyelitis, hematoma, diabetic muscle infarction, or soft tissue tumor.4
CONCLUSION
Diagnosing pyomyositis needs a high index of suspicion. In our case, the absence of fever and other signs of inflammation initially and negative ultrasound imaging of the thigh made the diagnosis challenging. Successful treatment requires early recognition, antibiotic therapy, imaging-guided aspiration, and debridement of affected tissues. This case highlights the need to have a high degree of suspicion and to recognize pyomyositis earlier, in patients who have thigh pain and mild skin changes even in the absence of fever, especially in patients who have diabetes, immunodeficient state, or viral infections.
REFERENCES
1. Ong CY, Lim JL, Galang LD, et al. Extensive pyomyositis of vastus muscle. Pan Afr Med J 2017; 28:30. DOI: 10.11.11604/pamj.2017.28.30.13544.
2. Annamalai AK, Gopalakrishnan C, Jesuraj M, et al. Pyomyositis. Postgrad Med J 2013;89(1049):179–180. DOI: 10.1136/postgradmedj-2012-131162.
3. Kumar MP, Seif D, Perera P, et al. Point of care ultrasound in diagnosing pyomyositis: A report of three cases. J Emerg Med 2014;47(4):420–426. DOI: 10.1016/j.jemermed.2014.02.002.
4. Comegna L, Guidone PI, Prezioso G, et al. Pyomyositis is not only a tropical pathology: A case series. J Med Case Rep 2016;10(1):372. DOI: 10.1186/s13256-016-1158-2.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.